Anterior temporal lobectomy and laser ablation for epilepsy: Comparing the impact on language and memory.
Abstract number :
3.345
Submission category :
Late Breakers
Year :
2013
Submission ID :
1865704
Source :
www.aesnet.org
Presentation date :
12/7/2013 12:00:00 AM
Published date :
Dec 5, 2013, 06:00 AM
Authors :
R. L. Rider, N. Taylor, P. Badkerhanian, M. Sperling, A. Sharan, J. Tinker, J. Tracy
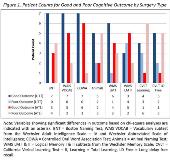
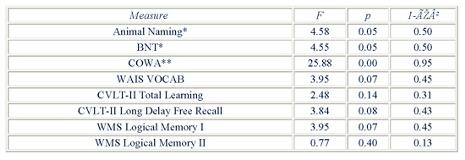
Rationale: Anterior temporal lobectomy (ATL) for temporal lobe epilepsy (TLE) has been associated with high rates of cognitive morbidity. Laser interstitial thermal therapy (LITT) is less invasive alternative to ATL that may reduce cognitive morbidity following surgery. Anecdotal evidence suggests LITT compares favorably to ATL in patients with similar seizure types. Here we provide the first empirical comparison of ATL and LITT on measures of expressive language and episodic memory, the cognitive domains most at risk in left TLE surgery. Methods: Well-established measures of intellectual ability, language, and episodic memory were administered to N=14 patients (age 23y 65y; 10f) with left TLE prior to either left ATL (n=7) or LITT (n=7) surgery. Groups were matched on age, sex, handedness, education, IQ, and presence of mesial temporal sclerosis. At one-month post- surgery, patients were re-assessed using alternate test forms when available. Indices of reliable change (RCI) for each cognitive measure were computed or taken from the literature. Change scores were calculated (post-surgical score pre-surgical score) and counted, based on the RCI cutoff values, as either a good (no change/ improvement) or poor outcome (significant decline). Chi square analysis was used to determine whether rates of good versus poor outcome were significantly different between the two surgical groups. Repeated measure ANOVA was used to test differences in the rate of change between ATL and LITT groups. Results: Language and memory performance did not differ significantly between groups at baseline (all p>.05). Chi-square analyses revealed significant differences between groups on measures of language (Boston Naming Test, p<.05) and episodic memory (California Verbal Learning Test-II, Long Delay Free Recall, p<.05) outcome, with LITT patients showing better outcomes across the majority of measures (see Fig.1). Repeated measures ANOVA revealed a significant interaction of test session (pre vs. post) by surgery type on measures of multiple language measures (see Table 1), with ATL patients showing significantly greater rates of decline than LITT patients. Both groups showed a pattern of decline in episodic memory, with a stronger downward trend for the ATL group, though rate of change was not significantly different between groups (all p>.07).Conclusions: To our knowledge, this is the first study to compare neurocognitive outcomes in patients undergoing left ATL versus LITT for seizure control. At one month post-surgery, LITT was associated with either stable language performance or significantly lower rates of decline than ATL, suggesting LITT, by impacting a smaller region of the temporal lobe, may preserve expressive language. The similar rate of decline on memory measures across the two groups is consistent with the notion that both procedures targeted the hippocampus, a structure critical for episodic memory encoding. Further research is needed to determine if the differences in outcome between these two interventions persist longitudinally.