Clinical Features and Outcomes of Psychogenic Nonepileptic Seizures: Results of Implementing a “Two-Way Care Model” in a Japanese Neuropsychiatry Setting
Abstract number :
1.268
Submission category :
6. Comorbidity (Somatic and Psychiatric)
Year :
2018
Submission ID :
496712
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Go Taniguchi, The University of Tokyo Hospital; Mao Fujioka, The University of Tokyo Hospital; Yumiko Okamura, The University of Tokyo Hospital; Kenichi Yano, The University of Tokyo Hospital; and Shinsuke Kondo, The University of Tokyo Hospital
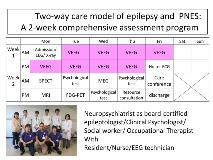
Rationale: It is recommended that mental health care providers be located within the Epilepsy Monitoring Unit (EMU) to achieve effective care in psychiatric comorbidities and psychogenic nonepileptic seizures (PNES). However, there has been little published literature regarding the influence of the involvement of mental health care providers within the EMU. Therefore, we evaluated the effectiveness of a “two-way care model” (meaning that neuropsychiatrists will diagnose and manage both epilepsy as well as PNES) in Japanese neuropsychiatry settings. Methods: The University of Tokyo Hospital Epilepsy Center is an academic medical institution and training facility of epileptologists accredited by the Japan Epilepsy Society. The neuropsychiatric, neurosurgical, and pediatric wards each have their own EMU for the medical treatment of epilepsy and related disorders. The EMU for the neuropsychiatric ward consists of the following major members: two neuropsychiatrists as board-certified epileptologists, one clinical psychologist, one social worker, and one occupational therapist. We are running a 2-week comprehensive assessment program, which includes 5 days of video-electroencephalographic monitoring, various neuroimaging tests, neuropsychiatric evaluations, and a care conference. In total, we retrospectively examined 88 patients (32 males; 56 females) who were admitted to the EMU of the neuropsychiatric ward of the University of Tokyo Hospital using case charts. Results: Twenty-one patients (23%) had PNES, and 16 patients (18%) had a dual diagnosis of PNES and epilepsy. The PNES group comprised 13 males (35%) and 24 females (65%). Five out of 37 patients with PNES (14%) reported previous sexual or physical abuse. Fourteen patients with PNES (38%) showed intellectual disabilities. Thirty-five patients with PNES (95%) continued treatment under the guidance of mental health providers (mean follow-up periods: 20.7 months ±11.5 SD). PNES disappeared in 16 (7 males; 9 females) of 24 patients (67%) who continued treatment at our hospital. Patients with PNES and epilepsy tended to have a better prognosis than patients with PNES alone. All 16 PNES-free patients could achieve the level of social life that they had before PNES onset, and moreover, 3 of these patients got a new job and their incomes also increased. Conclusions: This study suggests that our “two-way care model” has a certain beneficial effect on the management of PNES. A seamless transition from diagnosis to management, accompanied by the adoption of a multidisciplinary approach, may contribute not only to the effective treatment of PNES patients with various backgrounds, but also to the maintenance of treatment compliance. We plan to further study the factors that increase the therapeutic efficacy in such cases. Funding: The authors declare no conflicts of interest associated with this manuscript.
.tmb-.jpg?Culture=en&sfvrsn=38181230_0)