Impact of Anti-Epileptic Drug Polypharmacy Among People Living with Epilepsy
Abstract number :
2.270
Submission category :
7. Antiepileptic Drugs / 7D. Drug Side Effects
Year :
2018
Submission ID :
502101
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Katharine Ozenberger, University of Illinois at Chicago; Jessica Levy, University of Illinois at Chicago; and Dilip Pandey, University of Illinois at Chicago
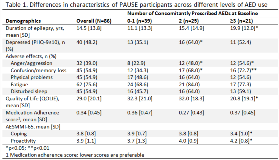
Rationale: Polypharmacy, the simultaneous use of multiple medications, is a growing public health concern among patients with chronic conditions. As the number of medications increase, so does the risk of adverse effects (AEs) that may place a significant burden on activities of daily living and quality of life. People living with epilepsy (PWE) are especially at risk given the potential mental health and cognitive AEs associated with anti-epileptic drugs (AEDs). Methods: We examine AED polypharmacy among PWE participating in PAUSE to Learn Your Epilepsy, an SM education effectiveness program that serves an underserved population. Demographic, clinical, and measures of SM skills were collected at baseline and compared across different levels of concomitant AED use. Quality of life in epilepsy was determined using the QOLIE-10-P questionnaire. Self-reported AEs and other impacts on daily living were also investigated. Descriptive statistics analyzed differences using Chi-square statistics or t-test, as appropriate. Results: We examined baseline data for 86 PAUSE participants: mean age was 37.7 years and 62.8% were female. Those who reported using =3 AEDs at baseline were more likely to be male, non-Hispanic white, and had a higher average age (40.9 years). Though not significant, individuals who take =3 AEDs also reported =2 comorbid chronic conditions and on average have had epilepsy longer. Participants who take =2 AEDs also reported a significantly higher prevalence of depressive symptoms within the previous two weeks and were more likely to report anger/aggression and confusion AEs. Notably, PWE who take =3 AEDs had a significantly lower quality of life and ability to cope with epilepsy. Conclusions: AED polypharmacy may be necessary to effectively manage epilepsy, yet represents a significant burden to psycho-emotional functioning in daily life. Patients who take =3 AEDs are more likely to report anger/aggression and confusion AEs, and lower SM skills for coping. However, PWE with =3 AEDs also had a higher proactivity score for medication, health care communication, and seizure safety. This underscores a group to focus on delivering SM education and skill-building. Funding: PAUSE is a project supported by the University of Illinois Prevention Research Center and the Centers for Disease Control and Prevention's MEW Network. The project is administered by the Institute for Health Research and Policy of the University of Illinois at Chicago, under CDC cooperative agreement no. U48-DP005010.