Implementation of an Inpatient Alert Protocol Reduces Time to Administration of Second-Line Antiseizure Medications for Status Epilepticus
Abstract number :
3.407
Submission category :
13. Health Services (Delivery of Care, Access to Care, Health Care Models)
Year :
2018
Submission ID :
488974
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Mauricio F. Villamar, University of Kentucky; Jordan L. Clay, University of Kentucky; Katelyn S. Dolbec, University of Kentucky; Aaron M. Cook, UK HealthCare Pharmacy Services; Chenlu Ke, University of Kentucky; Yan Xu, University of Kentucky; Rachel Ward
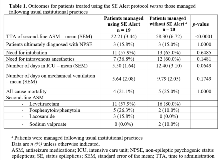
Rationale: A prior quality improvement study in our institution found that the mean time to administration (TTA) of a second-line anti-seizure medication (ASM) for patients in status epilepticus (SE) was 71±11.8 minutes. Delays in treatment failed to improve after an educational program for residents, pharmacists, and nursing staff, and the development of an electronic SE order set. Our objective was to determine whether the implementation of a SE Alert protocol improves TTA of a second-line ASM in hospitalized adults being treated for SE. Methods: We developed and implemented an inpatient SE Alert system (Fig. 1). A quasi-experimental cohort study was performed. We analyzed all patients aged 18-85 years who were managed at the University of Kentucky Medical Center using the SE Alert protocol between March 2015 and June 2017 (n=19). Controls were the first 20 consecutive patients treated for SE over the same time period, but who were managed following existing institutional practices (i.e., without SE Alert protocol).The primary outcome was TTA of a second-line ASM in patients for whom a SE Alert was initiated compared to control patients for whom a SE Alert was not initiated. Secondary outcomes included the need for intubation, administration of intravenous anesthetics, number of days in the intensive care unit (ICU), number of days on mechanical ventilation, and all-cause mortality during the index hospitalization. Results: Mean TTA of a second-line ASM was shorter with the use of the SE Alert system (22.21±3.44 minutes) compared to usual care (58.30±6.72 minutes; p<0.0001). There was a trend toward fewer days in ICU for patients managed with the SE Alert protocol. There were no differences between groups in the need for intubation, administration of intravenous anesthetics, number of days on mechanical ventilation, or all-cause mortality (Table 1). Conclusions: Implementation of a SE Alert system led to a marked improvement in TTA of a second-line ASM and to a trend toward shorter ICU stay for patients for whom it was used. Other secondary outcomes, including all-cause mortality, were not affected by the use of the SE Alert system. Future, larger randomized, multicenter studies would be helpful for determining the impact of the SE Alert system on patient outcomes. Funding: This study received no targeted funding.