Outcome of Epilepsy Patients Unsuitable for Resective Surgery Following Invasive Monitoring
Abstract number :
3.320
Submission category :
9. Surgery / 9A. Adult
Year :
2018
Submission ID :
496207
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Daniel B. Eddelman, Rush University Medical Center; Kavantissa Keppetipola, Rush University Medical Center; Fiona Lynn, Rush University Medical Center; Rebecca O'Dwyer, Rush University Medical Center; Rich Byrne, Rush University Medical Center; and Sepehr
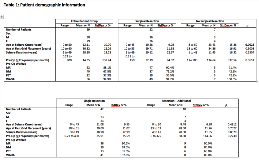
Rationale: Approximately 10-20% of patients with medically refractory epilepsy are candidates for resective surgery. When a resectable seizure focus is suspected but not confirmed by non-invasive testing, intracranial electrocorticography with depth or surface electrodes is recommended. Invasive monitoring has a high likelihood of identifying the seizure focus, but in 10-20% of cases, no resectable focus is identified. Furthermore, while seizure focus resection has been shown to result in good clinical and surgical outcomes, a small subset of patients may have inadequate seizure control and require further surgical intervention. This may be in the form of repeat intracranial electrode monitoring and further seizure focus resection, or responsive neurostimulation system (RNS) implantation. There is currently a lack of long-term outcomes evidence in regards to these patients who fail initial seizure focus resection and require a second surgical intervention. Herein we present our outcomes for patients who underwent invasive intracranial monitoring. Methods: Retrospective review of the electronic medical record was performed for all patients undergoing invasive (subdural or depth electrode) EEG monitoring between 2003 and 2017. These patients were split into two groups: those who progressed to seizure focus resection (“surgical resection”), and those who were found to be inappropriate for resective surgery (“no surgical resection”). The surgical resection group was further divided into two subgroups: those who required no additional surgical intervention (“single resection”), and those who required a second procedure in the form of either repeat intracranial monitoring and seizure focus resection or RNS placement (“resection+additional”).Data collected included patient demographics; length of seizure history; non-operative pre-operative workup; seizure focus location; reasons for lack of resection; length of follow-up; and seizure outcomes. Patients were excluded from outcomes analysis if they were lost to follow-up before 6 months. Length of follow-up was measured from the patient’s most recent surgical intervention. Results: Fifty-nine patients underwent invasive intracranial monitoring. Patient demographics are summarized in Table 1. Adequate follow-up data was available for 55 of the 59 patients. Follow-up data are summarized in Table 2.Intracranial electrode monitoring resulted in successful identification of seizure focus in a high percentage (88.1%) of patients in whom non-invasive workup was inconclusive. Of the 49 surgical group patients with sufficient follow-up data, 39 (79.6%) did not require further surgical intervention, and 28 (74.4%) achieved seizure freedom. Ten patients (20.4%) did not experience adequate seizure control even after intracranial monitoring and resection. Six of these patients underwent a second intracranial electrode monitoring procedure followed by repeat seizure focus resection, while 4 patients underwent RNS implantation. Interestingly, neither the latest follow-up seizure frequency nor the percent seizure reduction was statistically different from the patients who only required a single resective surgery. While only one patient ultimately achieved seizure freedom, the remaining 9 patients achieved Engel’s Class II. Conclusions: Our data suggests that in patients who fail seizure focus resection after intracranial monitoring, further surgical intervention (either repeat monitoring and resection or RNS placement) may be a viable option and can result in similar overall long-term outcomes to those patients who only require a single resective surgery. Funding: No funding was received.
.tmb-.png?Culture=en&sfvrsn=5f2df22d_0)