STEROID-RESPONSIVE EPILEPSIA PARTIALIS CONTINUA DUE TO PARANEOPLASTIC ENCEPHALITIS
Abstract number :
3.192
Submission category :
Year :
2005
Submission ID :
5998
Source :
www.aesnet.org
Presentation date :
12/3/2005 12:00:00 AM
Published date :
Dec 2, 2005, 06:00 AM
Authors :
Mandeep Garewal, Salvador Cruz, Jayant N. Acharya, and R. Edward Hogan
Epilepsy partialis continua (EPC) is rarely related to paraneoplastic syndromes. We present a case of EPC, refractory to multiple AEDs, which responded to treatment with methylprednisolone. We reviewed the findings of a 63 year old woman who presented with EPC. A 63 year old woman presented with EPC of the left hemi-face and arm of 3 weeks duration. Extensive workup including CSF results, cytology, herpes PCR, encephalitis panel, Lyme antibodies (abs), HIV abs and ELISA testing, was negative. Paraneoplastic panel was positive for anti-striatal abs.
AEDs (valproic acid, phenytoin, levetiracetam, carbamazepine, and chlorazepate) given in maximally-tolerated doses did not result in improvement of EPC. Propofol reduced the severity but did not abolish the EPC. Four weeks after onset of EPC, the patient was treated with methylprednisolone 250 mg IV q 6 hours.
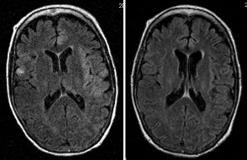
Neuroimaging was obtained 2 weeks before the onset of EPC and at weeks 3, 4, 5 after onset of EPC.
The day following methylprednisolone treatment, the seizure frequency and duration had remarkably diminished. Three days later, EPC had subsided. Methyl-prednisolone was administered for a total of 5 days, followed by a course of oral prednisone. Phenytoin, chlorazepate and valproate were weaned off. The patient was discharged on carbamazepine, levetiracetam and oral prednisone. Prednisone was tapered over the following two months. One year after presentation, she had no recurrence of symptoms. Five weeks after onset of EPC, a biopsy of a lung nodule showed small cell carcinoma, which prompted treatment with chemotherapy and radiation.
Neuroimaging findings: MR brain 2 weeks prior to EPC (obtained for clinical indication of encephalopathy) was normal. At 3 weeks after onset of EPC, FLAIR showed hyperintensity in the left frontal, temporal, and insular regions. At week 4 after EPC onset, an additional hyperintensity was noted in the right frontal region, which resolved on repeat MR obtained 5 weeks after EPC onset. There was no contrast enhancement at any time. The figure shows FLAIR images before and after steroid treatment of EPC. EPC is commonly refractory to conventional AEDs, but may respond to treatment with corticosteroids. Our case illustrates that corticosteroids can be efficacious in treating paraneoplastic-related EPC. Continued resolution of EPC after taper of corticosteroids was likely related to treatment of the underlying neoplasm. This case illustrates the importance of workup for associated neoplasm in patients with EPC.[figure1]