The Prevalence of Coexisting Epilepsy in Adult Patients With Psychogenic Non-Epileptiform Spells
Abstract number :
2.415
Submission category :
16. Epidemiology
Year :
2018
Submission ID :
502766
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Joseph Newman, Saint Luke's Hospital; Jennifer Dutton, Saint Luke's Hospital; Ronald Fields, Saint Luke's Hospital; and John Croom, Saint Luke's Hospital
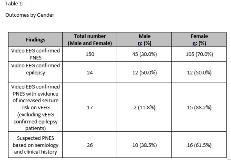
Rationale: Rationale: The aim of this study was to identify the prevalence of coexisting epilepsy in adults with a definitive diagnosis of psychogenic non-epileptiform spells (PNES) utilizing continuous video electroencephalography (vEEG) monitoring at our Level 4 Comprehensive Epilepsy Center. Methods: Methods: Data was collected on all patients who were admitted to the Saint Luke’s Marion Bloch Neuroscience Institute’s adult epilepsy monitoring unit (EMU), received vEEG monitoring, and were followed by a board certified epileptologist between June, 2016 and May, 2018. Patients with vEEG confirmed PNES and epilepsy, suspected PNES based on semiology and clinical history, and PNES with evidence of epileptiform discharges on EEG were retrospectively reviewed and compared. Results: Results: Out of 619 adults who underwent vEEG monitoring between June, 2016 and May, 2018, 150 (24.2%) patients were definitively diagnosed with PNES with vEEG monitoring. Of those adults, 105 (70.0%) were female and 45 (30.0%) were male. Twenty-four (16.0%) of the 150 patients with vEEG confirmed PNES also had epileptic seizures confirmed by vEEG or had evidence of an idiopathic primary generalized epilepsy condition (4 patients out of the 24). Seventeen (11.3%) patients who had vEEG confirmed PNES also had evidence of epileptiform discharges. While electrographic seizures were not captured on vEEG in those patients, it was suspected they had a significant likelihood of concomitant epilepsy based on their interictal vEEG findings. In addition to the 150 patients with vEEG confirmed PNES, 26 patients (4.2%) were thought to have a high suspicion of PNES based on semiology and clinical history, but their episodes were not captured on vEEG for a definitive diagnosis. Gender differences were compared in each of these categories (Table 1). Conclusions: Conclusions: Over a two-year period at our Level 4 Comprehensive Epilepsy Center, 150 (24.2% of 619) patients had vEEG confirmed PNES with an additional 26 patients having suspected PNES. Out of the 150 patients with vEEG confirmed PNES, 24 patients had vEEG confirmed epilepsy while an additional 17 patients had epileptiform abnormalities on their EEG. Thus, at our Comprehensive Epilepsy Center, a significant proportion of patients (27.3% or 41) with video EEG confirmed PNES had either video EEG proven concomitant epilepsy or an interictal EEG pattern highly suspicious for having concomitant epilepsy. Therefore, in patients with confirmed PNES, we recommend a thorough evaluation to assess for the presence of concomitant epilepsy. Funding: None